Air Pollution & Neurological Disorders: US Policy Implications
A new study unveils a significant link between air pollution and neurological disorders, raising urgent questions about its profound implications for current and future US environmental policy, particularly concerning public health and regulatory frameworks.
Recent scientific findings are reshaping our understanding of environmental health, particularly the insidious impact of airborne contaminants. A new study reveals a link between air pollution and neurological disorders: what are the implications for US environmental policy, and how might these findings necessitate a significant reevaluation of our protective measures?
The Emerging Science: Air Pollution’s Neurological Threat
The understanding of air pollution’s reach has expanded far beyond respiratory ailments. Breakthrough research is now clearly demonstrating a troubling connection between the microscopic particles we breathe and the delicate intricacies of our brain health. This evolving scientific landscape demands a closer look.
For decades, studies primarily focused on the cardiovascular and pulmonary impacts of air quality. However, advanced neuroimaging, molecular biology, and epidemiological studies are providing compelling evidence that the brain is not immune to these environmental aggressors.
Understanding the Pathways of Harm
How exactly do tiny particles in the air reach and affect the brain? Scientists are identifying several key mechanisms:
- Direct Translocation: Ultrafine particles (PM2.5 and smaller) can bypass the body’s usual defenses, entering the bloodstream directly from the lungs and traveling to the brain. They can also enter via the olfactory bulb, connecting directly to neural pathways.
- Systemic Inflammation: Inhaled pollutants trigger inflammatory responses throughout the body. Chronic systemic inflammation can compromise the blood-brain barrier, a protective shield, allowing harmful substances and inflammatory signals to penetrate the brain.
- Oxidative Stress: Air pollutants are rich in reactive oxygen species, leading to oxidative stress. This imbalance damages cells, including neurons, and can contribute to neurological degeneration.
The implications of these findings are profound. They suggest that what we once considered an external threat primarily affecting our lungs is, in fact, a pervasive systemic toxin with a direct line to our most vital organ. This necessitates a fundamental shift in how we perceive and regulate air quality.
Specific Neurological Disorders Implicated
While the initial links were observational, the latest research provides stronger evidence, correlating specific types of air pollution with an elevated risk or exacerbation of various neurological conditions. It’s not just a general malaise; specific conditions are showing statistical connections.
This growing body of evidence calls for urgent attention from public health officials and policymakers alike, as the scope of potential harm appears more extensive than previously understood.
Alzheimer’s Disease and Dementia
Several long-term studies have identified a consistent link between exposure to fine particulate matter (PM2.5) and an increased risk of developing Alzheimer’s disease and other forms of dementia. Researchers propose that chronic inflammation and oxidative stress induced by pollutants contribute to the accumulation of amyloid plaques and tau tangles, hallmarks of Alzheimer’s.
Parkinson’s Disease
Recent meta-analyses indicate a correlation between long-term exposure to certain air pollutants, including PM2.5 and nitrogen dioxide (NO2), and a higher prevalence of Parkinson’s disease. The exact mechanisms are still being explored, but neuroinflammation and mitochondrial dysfunction are key suspects.
Stroke and Cerebrovascular Events
- Increased Risk: Short-term and long-term exposure to various air pollutants is consistently associated with an elevated risk of ischemic stroke.
- Mechanisms: Pollutants can promote arterial stiffness, increase blood pressure, and contribute to the formation of blood clots, all factors that raise stroke risk.
- Cognitive Decline: Even non-fatal strokes or silent cerebrovascular damage can contribute to cognitive impairment over time.
The range of neurological conditions potentially impacted by air pollution underscores the complexity of this environmental health challenge. These aren’t isolated incidents but rather signs of a broader, systemic threat that requires a multi-faceted response.
Current US Environmental Policy Landscape
The United States has a robust, albeit continuously debated, framework for environmental protection. Key legislation and agencies aim to safeguard public health from various environmental hazards. Understanding the existing policy landscape is crucial before proposing future changes.
The primary legislative cornerstone for air quality control is the Clean Air Act (CAA), first enacted in 1970 and significantly amended in 1977 and 1990. This act empowers the Environmental Protection Agency (EPA) to set national air quality standards.
The Clean Air Act (CAA) and EPA
The CAA established National Ambient Air Quality Standards (NAAQS) for six common air pollutants, known as criteria pollutants:
- Particle pollution (particulate matter, including PM2.5 and PM10)
- Ground-level ozone
- Carbon monoxide
- Sulfur oxides
- Nitrogen oxides
- Lead
Under the CAA, the EPA regularly reviews the scientific literature to determine if current NAAQS are sufficiently protective of public health. States are then responsible for developing State Implementation Plans (SIPs) to meet or maintain these standards, with enforcement mechanisms in place.
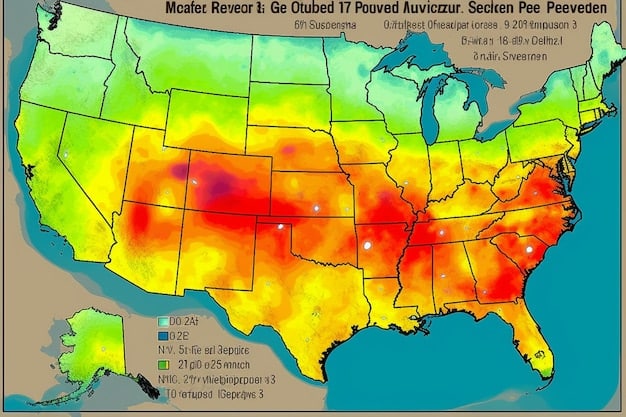
Challenges and Debates
Despite the CAA’s successes in reducing overall air pollution levels, significant challenges persist. Debates often arise regarding the stringency of NAAQS, the economic impact of regulations, and the pace of enforcement. Environmental justice concerns also highlight that marginalized communities often bear a disproportionate burden of exposure to pollutants.
As new scientific evidence emerges, particularly concerning neurological impacts, these debates become even more pressing, pushing the boundaries of what existing policies can effectively address.
Implications for US Environmental Policy
The undeniable link between air pollution and neurological disorders presents critical new considerations for US environmental policy. This isn’t merely about tweaking existing regulations; it’s about fundamentally reassessing what “public health” means in the context of air quality.
The traditional focus on respiratory and cardiovascular health, while important, now appears incomplete. Policy must evolve to encompass the brain’s vulnerability.
Revisiting National Ambient Air Quality Standards (NAAQS)
The current NAAQS for particulate matter have primarily considered respiratory and cardiovascular effects. With neurological impacts now firmly established, the EPA will need to:
- Strengthen PM2.5 Standards: The evidence suggests that even current “safe” levels of PM2.5 may not be protective enough for brain health. Lowering the primary standards could become a public health imperative.
- Consider New Pollutants: Research might uncover neurological impacts from pollutants not currently designated as criteria pollutants, necessitating their inclusion or stricter regulation.
- Review Other Criteria Pollutants: The neurological effects of other criteria pollutants, like nitrogen oxides and ozone, may also warrant a re-evaluation of their respective NAAQS.
Such revisions would trigger significant shifts in state implementation plans, potentially affecting industries, transportation, and urban planning. The costs of action must be weighed against the immense societal burden of neurological diseases.
Enhanced Public Health Initiatives and Research Funding
Beyond regulatory adjustments, a more proactive public health strategy is needed:
- Increased Monitoring: Expanding air quality monitoring networks, especially in vulnerable communities, will provide more granular data for targeted interventions.
- Public Awareness Campaigns: Educating the public about the neurological risks of air pollution can empower individuals to take protective measures.
- Research Investment: Sustained funding for research into the precise mechanisms of neurotoxicity, long-term epidemiological studies, and effective intervention strategies is crucial. This includes funding for studies on vulnerable populations, such as children and the elderly.
The intersection of environmental health and neurology demands a comprehensive, science-driven policy response that transcends traditional regulatory boundaries. It calls for foresight and a commitment to protecting the most sensitive organ in the human body.
Economic and Societal Considerations
Implementing stricter environmental policies in response to the neurological impacts of air pollution comes with significant economic and societal implications. These aren’t just scientific challenges; they are complex socio-economic puzzles requiring careful balancing acts.
Any policy shift must consider the costs of compliance for industries, potential impacts on economic growth, and the broader societal benefits of improved public health. The scale of neurological disorders represents an enormous economic burden.
Cost of Illness vs. Cost of Prevention
Treating neurological disorders, from dementia to Parkinson’s, involves immense healthcare costs, lost productivity, and familial burdens. These indirect costs often far outweigh the direct medical expenses.
- Healthcare Burden: Increased rates of neurological conditions strain healthcare systems, leading to higher insurance premiums and public health expenditures.
- Economic Productivity: Cognitive decline and neurological impairment reduce workforce participation and overall economic output.
- Caregiver Strain: Families often bear the brunt of caregiving, affecting their own well-being and economic participation.
From an economic perspective, investing in cleaner air—by modernizing energy infrastructure, promoting electric vehicles, and improving industrial emissions controls—could yield substantial long-term savings by reducing the incidence and severity of these debilitating diseases. This argument strengthens the case for preventative measures.

Impacts on Industry and Innovation
Stricter regulations typically mean industries must invest in new technologies and processes to reduce emissions. While this can initially be seen as a burden, it also drives innovation.
- Technological Advancement: Demand for cleaner technologies stimulates research and development, creating new industries and jobs.
- Market Competitiveness: Companies that embrace sustainable practices can gain a competitive edge in a global market increasingly prioritizing environmental responsibility.
- Green Economy Growth: Policies that incentivize renewable energy and efficient resource use contribute to the growth of a “green economy.”
Navigating these complex economic and societal considerations requires transparent dialogue, accurate cost-benefit analyses, and innovative policy designs that foster both environmental protection and sustainable economic development. The long-term health and economic well-being of the nation depend on making well-informed choices.
Future Policy Directions and Public Engagement
The unfolding science linking air pollution to neurological disorders necessitates not just an adjustment but a proactive evolution of US environmental policy. This journey will require a multi-pronged approach, drawing on technological innovation, interagency cooperation, and robust public engagement to build a healthier future.
Our goal must be to move beyond reactive measures towards a preventative paradigm, truly safeguarding the brain health of current and future generations.
Integrated Policy Approaches
No single policy change will be sufficient. Future strategies will likely involve:
- Cross-Agency Collaboration: Greater coordination between the EPA, CDC (Centers for Disease Control and Prevention), NIH (National Institutes of Health), and transportation and urban planning departments is essential to address the complex nature of this issue.
- “Source-to-Brain” Strategy: Policies need to consider the entire pathway of pollutants, from industrial emissions and vehicle exhaust to their eventual impact on human neurological systems.
- Smart City Initiatives: Promoting urban planning that prioritizes green spaces, public transport, and reduced vehicle emissions can create healthier living environments. This includes incentives for sustainable building materials and practices.
The challenge is immense, but the opportunity to prevent widespread neurological damage is even greater. This requires thinking beyond traditional environmental silos.
The Role of Public Engagement and Advocacy
Public awareness and sustained advocacy will be critical drivers of policy change. Citizens, health professionals, and environmental groups have a vital role to play in:
- Educating Communities: Disseminating clear, accessible information about the risks and preventative measures is crucial.
- Supporting Policy Changes: Grassroots movements can amplify the call for stronger regulations and increased funding for research.
- Demanding Accountability: Holding polluters and policymakers accountable for environmental health outcomes reinforces the public health imperative.
Ultimately, addressing the neurological threat posed by air pollution is a collective responsibility. It demands that we not only understand the science but also translate that understanding into decisive action, shaping a cleaner, healthier future for all Americans.
| Key Aspect | Brief Description |
|---|---|
| 🧠 Neurological Link | New studies confirm air pollution’s role in brain disorders like Alzheimer’s and Parkinson’s. |
| ⚖️ Policy Implications | Demands stricter NAAQS, expanded monitoring, and increased research funding. |
| 💰 Economic Impact | Prevention costs may be offset by significant savings from reduced healthcare burden of neurological diseases. |
| 🗣️ Public Role | Public awareness and advocacy are crucial for driving policy reform and accountability. |
Frequently Asked Questions
▼
Recent studies suggest strong links between air pollution exposure and an increased risk of developing or exacerbating conditions such as Alzheimer’s disease, various forms of dementia, Parkinson’s disease, and cerebrovascular events like stroke. The fine particulate matter (PM2.5) is often cited as a primary culprit due to its ability to bypass the body’s defenses and induce systemic inflammation and oxidative stress that damage brain cells.
▼
Air pollutants can affect the brain through several pathways. Ultrafine particles can directly enter the bloodstream via the lungs, travel to the brain, and even enter directly through the olfactory nerve. Additionally, air pollution triggers widespread inflammation in the body, which can compromise the blood-brain barrier, allowing harmful substances and inflammatory signals to penetrate the brain, leading to neuronal damage.
▼
The new findings put pressure on US environmental policy, particularly the Clean Air Act and EPA’s National Ambient Air Quality Standards (NAAQS). There’s a strong argument for reassessing and potentially strengthening current PM2.5 standards, potentially including new pollutants, and increasing funding for research into neurotoxic effects. Policies may need to shift from solely focusing on respiratory health to a more comprehensive “source-to-brain” approach.
▼
Yes, it’s highly probable. As scientific evidence solidifies the link between air pollution and severe neurological conditions, the EPA will face increasing pressure to revise and potentially lower existing air quality standards, especially for particulate matter. This would necessitate more stringent emissions controls across various sectors, including transportation and industry, aligning policy with the latest understanding of public health risks.
▼
Public engagement is crucial. Citizens can advocate for stronger environmental policies, support research initiatives, and participate in community efforts to reduce local pollution sources. Raising awareness about the neurological risks of air pollution among family, friends, and community members can also help build a collective demand for cleaner air. Informed and active public participation is essential for driving policy change.
Conclusion
The emerging scientific consensus on the link between air pollution and neurological disorders marks a pivotal moment for public health and environmental policy in the United States. No longer can we view air quality solely through the lens of respiratory or cardiovascular health; the brain’s vulnerability demands an urgent, comprehensive reassessment of our regulatory frameworks. As we move forward, integrating these profound neurological implications into policy decisions will be paramount, fostering a future where clean air truly means a healthy brain and a resilient society.





