Human Microbiome Project: Gut Health Innovations in US (Last 3 Months)
Recent findings from the Human Microbiome Project in the last three months reveal significant advancements in understanding gut health’s profound impact on various physiological systems in the US, highlighting novel pathways for therapeutic interventions and personalized nutrition strategies.
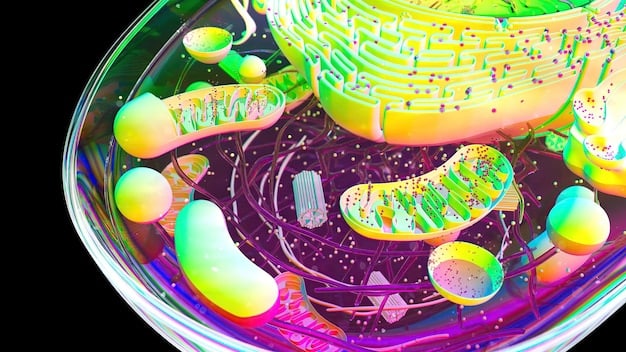
The human gut, often referred to as our “second brain,” harbors a bustling ecosystem of microorganisms profoundly influencing our health. For scientists and healthcare professionals across the United States, keeping pace with the rapid advancements in this field is crucial. The Human Microbiome Project: What New Insights Have Emerged in the Last 3 Months Regarding Gut Health in the US? is not just an academic question; it represents a frontier of medical discovery constantly pushing the boundaries of our understanding.
deciphering the microbiome: a dynamic landscape
The Human Microbiome Project (HMP), initially launched in 2007, fundamentally shifted our understanding of human biology by cataloging the microbial communities residing within and on us. What began as a foundational mapping effort has evolved into a dynamic research endeavor, with new insights emerging constantly. The past three months have been particularly fruitful, with a concentrated focus on how these microscopic inhabitants influence diverse aspects of gut health in the US population.
Current research efforts are moving beyond mere identification to functional analysis, exploring not just “who” is there, but “what” they are doing. This includes investigating metabolic pathways, host-microbe interactions, and environmental influences that shape the gut ecosystem. Understanding these complex dynamics is paramount for developing targeted interventions.
advances in personalized nutrition
One of the most exciting areas seeing significant progress is personalized nutrition, driven by microbiome data. Researchers are increasingly identifying specific microbial signatures that correlate with individual responses to diet. This paves the way for dietary recommendations tailored to an individual’s unique gut flora, moving beyond generalized advice.
- Dietary Fiber and Butyrate Production: New studies are refining our understanding of how different types of dietary fibers modulate the gut microbiome to produce short-chain fatty acids like butyrate, crucial for gut barrier integrity and anti-inflammatory responses.
- Protein Fermentation and Metabolite Profiles: Investigations into the impacts of protein sources on gut microbiota are revealing how amino acid fermentation by specific bacteria can yield beneficial or detrimental metabolites, influencing metabolic health.
- Prebiotic and Probiotic Efficacy: The efficacy of various prebiotics and probiotics is being re-evaluated through more rigorous human trials, leading to a clearer picture of which strains and compounds are most beneficial for specific gut health conditions.
These findings are not merely academic; they have direct implications for public health initiatives and dietary guidelines. The emphasis is shifting towards fostering a diverse and resilient microbiome through conscious dietary choices, rather than a one-size-fits-all approach.
The integration of artificial intelligence and machine learning is accelerating these discoveries, allowing for the analysis of vast datasets correlating dietary intake, microbiome composition, and health outcomes. This analytical power is revealing previously unseen patterns and predictive markers, essential for moving personalized nutrition from theory to practice in clinical settings across the US.
gut-brain axis: novel connections and therapeutic targets
The intricate bidirectional communication between the gut and the brain, known as the gut-brain axis, continues to be a hotbed of research. Recent findings have further solidified the role of the microbiome in influencing neurological and psychological states, offering new avenues for understanding and treating a range of disorders prevalent in the US.
Studies are elucidating the specific microbial metabolites and neurotransmitters that act as messengers between the gut and the brain. This includes exploring the roles of serotonin, dopamine, and GABA production by gut bacteria, and how dysbiosis can disrupt these crucial signaling pathways. The implications for mental health are profound, suggesting that gut-targeted therapies could complement traditional approaches.
microbial influence on neurological disorders
The past three months have seen compelling data linking specific microbiome profiles to neurological conditions. Research focusing on neurodegenerative diseases such as Parkinson’s and Alzheimer’s is gaining momentum, with preclinical and early clinical studies pointing to a causal role of gut dysbiosis in disease progression.
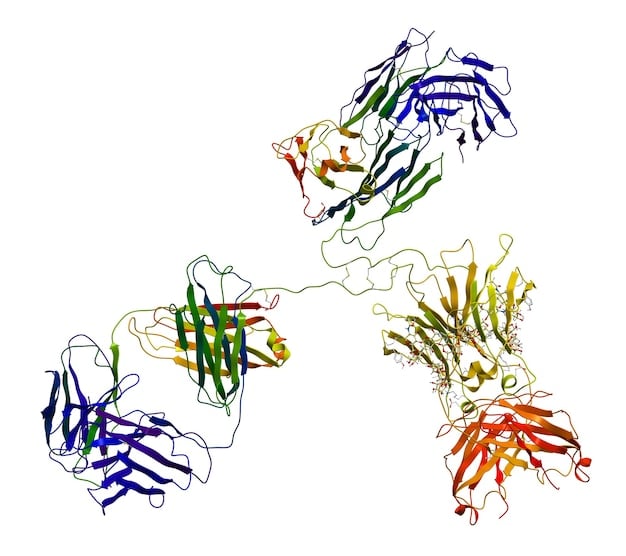
- Parkinson’s Disease and Alpha-Synuclein: New evidence suggests that certain gut bacteria might produce compounds that influence the aggregation of alpha-synuclein, a protein implicated in Parkinson’s. This opens the door for microbiome modulation as a preventative or therapeutic strategy.
- Alzheimer’s Disease and Neuroinflammation: Studies are detailing how gut microbiota dysregulation can contribute to systemic inflammation, which in turn crosses the blood-brain barrier, fueling neuroinflammation observed in Alzheimer’s patients.
Furthermore, the connection between the microbiome and mood disorders, including anxiety and depression, is being explored with renewed vigor. Researchers are investigating how probiotic interventions or dietary changes aimed at rebalancing the gut flora can lead to improvements in mood and cognitive function, providing hope for millions affected by these conditions in the US.
The development of psychobiotics – beneficial bacteria with mental health benefits – represents a pioneering frontier. Though still in early stages, the potential for novel treatments for depression and anxiety, specifically those targeting the gut microbiome, is immensely promising. This multidisciplinary approach, bridging gastroenterology, neurology, and psychiatry, underscores the complexity and interconnectedness of human health.
inflammatory bowel diseases: new diagnostic and therapeutic avenues
For individuals suffering from Inflammatory Bowel Diseases (IBD), which include Crohn’s disease and ulcerative colitis, the prospect of new diagnostic markers and therapeutic options is a beacon of hope. Recent microbiome research has provided breakthroughs in understanding the pathogenesis of these chronic conditions, which affect a significant portion of the US population.
Specifically, new studies have identified distinct microbial signatures associated with IBD onset and flare-ups. This includes a reduction in beneficial bacteria and an increase in pro-inflammatory species. These findings are crucial for developing non-invasive diagnostic tools that could allow for earlier detection and more personalized treatment strategies.
microbiome-targeted therapies for ibd
The shift towards microbiome-targeted therapies represents a paradigm shift in IBD management. Rather than solely focusing on suppressing inflammation, researchers are now exploring interventions that aim to restore microbial balance and promote gut healing. This includes the exploration of advanced fecal microbiota transplantation (FMT) techniques and novel probiotic formulations.
- Next-Generation Probiotics: The development of highly specific, live biotherapeutic products (LBP) designed to introduce beneficial strains that are deficient in IBD patients is showing promise. These are more targeted than traditional probiotics and are being rigorously tested for safety and efficacy.
- Dietary Interventions: Tailored dietary strategies, such as specific carbohydrate diets or elimination diets, are being investigated for their ability to modify the gut microbiome in ways that reduce inflammation and alleviate IBD symptoms.
- Metabolite-Based Therapies: Beyond microbes themselves, researchers are isolating and utilizing specific microbial metabolites (e.g., short-chain fatty acids) that exert anti-inflammatory effects within the gut. These metabolites could potentially be administered directly as therapeutic agents.
The long-term goal is to move towards precision medicine for IBD, where treatment is determined by an individual’s unique microbiome profile. This approach promises to reduce side effects and improve patient outcomes significantly. The collaborative efforts between academic institutions and pharmaceutical companies are accelerating the translation of these research findings into clinical practice.
Furthermore, understanding the interplay between genetic predispositions and environmental factors, molded by the microbiome, is shedding light on why certain individuals develop IBD while others do not. This holistic view is crucial for both prevention and treatment strategies.
obesity and metabolic syndrome: re-evaluating microbial roles
The increasing prevalence of obesity and metabolic syndrome in the US continues to be a major public health concern. Recent microbiome research has deepened our understanding of how gut bacteria contribute to energy harvest, fat storage, and insulin sensitivity, offering new targets for intervention.
New data highlights the contribution of specific microbial communities to the efficiency with which calories are extracted from food. Certain gut microbial profiles are associated with higher rates of energy harvest, meaning individuals with these profiles might extract more calories from the same amount of food, contributing to weight gain.
microbial influence on satiety and metabolism
Beyond energy extraction, the gut microbiome influences host metabolism through complex signaling pathways affecting appetite regulation, glucose homeostasis, and lipid metabolism. Researchers are identifying specific bacterial species and their metabolites that directly impact these processes. This includes discussions on how the microbiome affects the production of hormones like GLP-1 and peptide YY, which influence satiety and glucose regulation.
- Bile Acid Metabolism: New insights illustrate how gut bacteria modify bile acids, which act as signaling molecules that influence host metabolism, including glucose and lipid regulation. Manipulating these pathways could offer therapeutic benefits.
- Branched-Chain Amino Acids: Increased levels of branched-chain amino acids (BCAAs), often associated with insulin resistance, are being linked to specific gut microbial activities. This suggests that modulating the gut flora could impact BCAA levels and improve insulin sensitivity.
- Gut Permeability and Endotoxemia: The role of dysbiosis in increasing gut permeability (leaky gut) and facilitating the translocation of bacterial endotoxins into the bloodstream is being better understood. This low-grade inflammation can contribute to systemic insulin resistance and other metabolic derangements.
These discoveries are paving the way for novel therapeutic approaches that target the microbiome to combat obesity and metabolic syndrome. This could involve probiotic interventions to introduce beneficial bacteria, prebiotic strategies to feed existing beneficial microbes, or even dietary patterns designed to shift the microbial composition towards a healthier state. The ultimate goal is to offer more sustainable and effective weight management solutions beyond conventional approaches.
The precise mechanisms by which specific microbial strains influence host physiology are being meticulously dissected. This includes advanced genetic sequencing and metabolomics to identify key bacterial genes and metabolites involved in metabolic regulation, allowing for highly targeted interventions. The complexities of this interplay mean that a multi-faceted approach will likely be required to yield significant clinical benefits.
advancements in gut microbiome sequencing and analysis
The past three months have witnessed remarkable progress not just in the findings themselves, but in the methodologies used to generate them. Advances in gut microbiome sequencing and bioinformatic analysis are making research more robust, comprehensive, and accessible, driving the field forward at an unprecedented pace within the US scientific community.
Next-generation sequencing (NGS) technologies continue to evolve, offering higher resolution and deeper insights into microbial communities. This includes an increased adoption of metagenomic sequencing, which provides information on the functional potential of the entire microbial community by sequencing all DNA present in a sample, rather than just marker genes.
enhanced analytical tools and databases
Beyond raw sequencing data, the development of sophisticated bioinformatic tools and reference databases has been critical. These tools enable researchers to process vast amounts of genomic data, identify microbial species with greater accuracy, and predict their metabolic capabilities. The integration of multi-omics data (e.g., metagenomics, metabolomics, metatranscriptomics) is painting a more complete picture of microbial activity.
- Improved Reference Genomes: Continuous efforts to expand and refine reference genome databases for gut microbes are enhancing the precision of taxonomic classification and functional annotation, allowing for more confident identification of novel species and their roles.
- Machine Learning for Predictive Modeling: The application of machine learning algorithms is transforming how researchers analyze complex microbiome datasets. These algorithms can identify subtle patterns and correlations, leading to predictive models for disease risk, treatment response, and optimal dietary strategies.
- Standardization of Protocols: A concerted effort to standardize sample collection, processing, and sequencing protocols across different research labs is improving data comparability and reproducibility, which are essential for building a reliable body of evidence in the field.
The accessibility of these advanced techniques is empowering a wider range of researchers, from academic institutions to biotech startups, to contribute to the field. This democratized access to powerful analytical tools is accelerating the discovery pipeline, translating basic research into applicable knowledge at a faster rate than ever before. The emphasis on data sharing and collaborative platforms is also amplifying the impact of individual studies.
These technological leaps are not just about collecting more data; they are about extracting more meaningful insights from the data. The capacity to integrate diverse biological datasets now allows scientists to connect the dots between microbial presence, microbial function, and host health outcomes with unprecedented clarity, leading to a more holistic understanding of gut health.
challenges and future directions for microbiome research
Despite the rapid progress, the field of gut microbiome research faces significant challenges. The complexity of the microbial ecosystem, inter-individual variability, and the influence of lifestyle factors present hurdles that researchers in the US are actively addressing. Overcoming these challenges is crucial for translating current insights into effective clinical applications.
One major challenge is the sheer diversity and individuality of the human microbiome. Each person’s microbiome is unique, influenced by genetics, diet, lifestyle, environment, and medication. This high degree of variability makes it difficult to establish universal microbial markers for health or disease, complicating the development of standardized treatments.
bridging the gap: from discovery to application
Another critical challenge lies in bridging the gap between scientific discovery and clinical application. While fascinating correlations are continually being uncovered, demonstrating a causal link and developing safe and effective microbiome-targeted therapies requires rigorous, well-controlled clinical trials. The regulatory landscape for such novel therapies is also evolving.
- Causation vs. Correlation: Differentiating between microbial changes that are a cause versus a consequence of a disease remains a significant hurdle. Longitudinal studies and mechanistic experiments are essential to establish causality.
- Standardization of Interventions: Developing standardized, regulated microbiome interventions—whether probiotics, prebiotics, or FMT—is complex due to the living nature of the therapeutics and the variability of their effects across individuals.
- Ethical and Societal Implications: As microbiome science advances, it raises ethical considerations regarding data privacy, genetic manipulation of microbes, and equitable access to novel microbiome-based diagnostics and therapies.
Looking ahead, future directions for microbiome research in the US involve a continued emphasis on large-scale cohort studies to capture population-level variations, coupled with deep mechanistic studies to understand microbial interactions at the molecular level. This integrated approach will be vital for developing truly personalized and effective health interventions.
The development of dynamic models that can predict how the microbiome responds to various interventions (e.g., diet, drugs) will also be crucial. This involves not only understanding the microbial community’s composition but also its metabolic outputs and interactions with the host immune system. International collaborations are also key to pooling resources and diversifying research cohorts, enhancing the generalizability of findings.
| Key Insight | Brief Description |
|---|---|
| 🔬 Personalized Nutrition | Advances in tailoring diets based on individual gut microbe profiles for optimized health outcomes. |
| 🧠 Gut-Brain Axis Progress | New connections revealed between gut microbes and neurological/psychological states. |
| 💊 IBD Therapies | Emerging microbiome-targeted diagnostics and treatments for Inflammatory Bowel Diseases. |
| 🧬 Tech Advancements | Significant leaps in sequencing methods and bioinformatic analysis tools bolstering research. |
frequently asked questions about the human microbiome
▼
The human microbiome refers to the collective genetic material of all microorganisms living in and on our bodies, with a vast majority residing in the gut. It’s crucial for gut health because these microbes play vital roles in digestion, nutrient absorption, immune system development, and protection against pathogens, directly influencing our overall well-being. A balanced microbiome is key to a healthy gut.
▼
Diet is one of the most powerful determinants of gut microbiome composition and function. Different foods provide specific nutrients that favor the growth of certain bacterial species. For example, high-fiber diets promote beneficial bacteria that produce short-chain fatty acids, while diets high in processed foods and sugar can foster less desirable microbial communities, impacting gut health negatively.
▼
Absolutely. Research into the gut microbiome is actively exploring new therapeutic strategies for a wide range of conditions, including inflammatory bowel diseases, obesity, metabolic syndrome, and even neurological disorders. By understanding how microbial imbalances contribute to disease, scientists aim to develop targeted interventions such as precision probiotics, prebiotics, and fecal microbiota transplants to restore health.
▼
Psychobiotics are probiotics that, when ingested, may produce mental health benefits through interactions with the gut-brain axis. They are specific strains of beneficial bacteria capable of influencing brain function and mood by producing neurotransmitters, modulating inflammation, or affecting neuronal pathways. While still a nascent field, psychobiotics hold promise for complementary treatments for anxiety, depression, and stress-related conditions.
▼
Technological advancements, particularly in next-generation sequencing and bioinformatics, are revolutionizing microbiome research. These tools allow scientists to accurately identify microbial species, analyze their genetic makeup, and predict their metabolic functions within the gut. Machine learning and AI are also enabling researchers to process vast datasets, uncovering complex patterns and correlations between microbial profiles and host health with unprecedented speed and accuracy.

conclusion
In the continually evolving landscape of health and wellness, the human gut microbiome stands out as a uniquely influential, albeit complex, frontier. The insights gleaned over just the past three months, particularly within the scientific community in the US, underscore the profound impact of this internal ecosystem on everything from personalized nutrition to neurological function and chronic disease management. While challenges remain in translating these discoveries into universal clinical applications, the trajectory of research is undeniably promising. The ongoing commitment to unraveling the mysteries of our microbial inhabitants holds the key to unlock new paradigms in preventive care, diagnostics, and therapeutic interventions, ultimately fostering a healthier future for individuals across the nation.





