The Science of Addiction: Unveiling Neural Mechanisms of Substance Abuse

The science of addiction explores the complex neural mechanisms underlying substance abuse, revealing how drugs alter brain function and drive compulsive behaviors. Understanding these processes is crucial for developing effective treatments and prevention strategies.
Addiction is a complex and pervasive issue that affects millions worldwide. But what exactly happens in the brain that turns casual substance use into a compulsive need? The science of addiction: Understanding the neural mechanisms underlying substance abuse is crucial for developing effective prevention and treatment strategies. By delving into the intricate workings of the brain, we can better understand how addiction takes hold and how we can combat its devastating effects.
Decoding the Addicted Brain: An Introduction to Neural Pathways
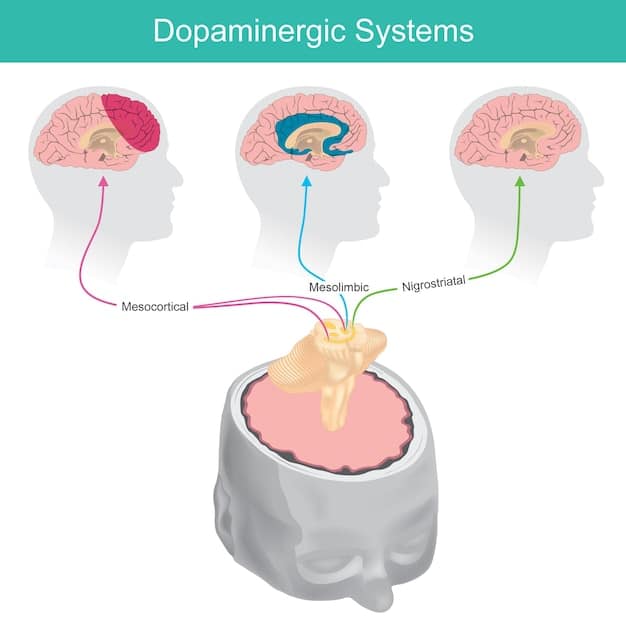
To truly grasp the science of addiction: Understanding the neural mechanisms underlying substance abuse, we must first explore the key brain regions involved. The mesolimbic dopamine system, often referred to as the “reward pathway,” plays a pivotal role in reinforcing behaviors, both natural and drug-induced. This pathway connects the ventral tegmental area (VTA) to the nucleus accumbens, releasing dopamine in response to pleasurable stimuli.
The Role of Dopamine in Addiction
Dopamine, a neurotransmitter, acts as a chemical messenger, transmitting signals between nerve cells in the brain. When we experience something pleasurable, such as eating a delicious meal or spending time with loved ones, dopamine is released, creating a sense of satisfaction and reinforcing the behavior. However, drugs of abuse hijack this system, causing a surge of dopamine far greater than that produced by natural rewards. This intense dopamine rush creates a powerful positive association with the drug, making it highly reinforcing and driving the user to seek out the experience repeatedly.
Furthermore, repeated drug use can lead to long-term changes in the brain’s dopamine system. The brain adapts to the excessive dopamine levels by reducing the number of dopamine receptors or decreasing dopamine production. This phenomenon, known as downregulation, results in a diminished response to natural rewards, making drugs even more appealing. The individual may experience a persistent feeling of emptiness or dissatisfaction, further fueling the addiction cycle.
- Drugs cause a dopamine surge, creating an intense positive association.
- Repeated drug use can lead to downregulation of dopamine receptors.
- Diminished response to natural rewards contributes to the addiction cycle.
In summary, the intricate interplay between dopamine and the brain’s reward system lies at the epicenter of the science of addiction. Understanding this dynamic is critical for developing targeted interventions that aim to restore the balance of dopamine levels and enhance the brain’s response to natural rewards.
The Neurobiology of Craving and Withdrawal
Beyond the initial euphoria, addiction involves a complex interplay of neurobiological processes that contribute to craving and withdrawal. These factors lock individuals into a cycle of dependence. The amygdala, a brain region involved in emotional processing, plays a key role in associating drug-related cues with intense cravings.
The Impact of the Amygdala
The amygdala can become hypersensitized to environmental cues associated with drug use, such as drug paraphernalia, specific locations, or even social settings. When exposed to these cues, the amygdala triggers powerful cravings and urges to use the drug. These cravings can be incredibly intense and difficult to resist, often leading to relapse even after periods of abstinence.
During withdrawal, the brain experiences a state of dysregulation as it attempts to adapt to the absence of the drug. This can result in a range of unpleasant symptoms, including anxiety, depression, insomnia, muscle aches, and nausea. These withdrawal symptoms can be so severe that individuals continue to use drugs simply to avoid the discomfort. Furthermore, chronic drug use can disrupt the brain’s stress response system, making individuals more vulnerable to stress and increasing the likelihood of relapse in response to stressful situations.
- The amygdala associates drug-related cues with intense cravings.
- Withdrawal symptoms can be severe and difficult to manage.
- Chronic drug use disrupts the brain’s stress response system.
In essence, craving and withdrawal are key components of the science of addiction, representing the body’s attempt to re-establish equilibrium in the absence of the drug. By understanding the underlying neural mechanisms of these phenomena, researchers can develop more effective treatments that target both the psychological and physiological aspects of addiction.
Executive Function and Impaired Decision-Making in Addiction
The prefrontal cortex, responsible for executive functions such as planning, decision-making, and impulse control, is significantly affected by chronic substance abuse. This impairment contributes to the hallmark behaviors of addiction, including continued drug use despite negative consequences. The science of addiction: Understanding the neural mechanisms underlying substance abuse also involves examining the impact on these critical cognitive functions.
Disruption of the Prefrontal Cortex
The prefrontal cortex exerts top-down control over impulses and desires, allowing individuals to weigh the long-term consequences of their actions. However, chronic drug use can weaken the prefrontal cortex, diminishing its ability to effectively regulate behavior. This can lead to impulsive decision-making, impaired judgment, and difficulty resisting drug cravings. Individuals may struggle to prioritize important life goals, such as maintaining relationships, holding down a job, or staying healthy, instead prioritizing the immediate gratification of drug use.
Moreover, addiction can lead to a phenomenon known as “cognitive inflexibility,” making it difficult for individuals to adapt to changing circumstances or shift their attention away from drug-related thoughts and behaviors. This lack of flexibility can make it challenging to engage in alternative activities or develop coping mechanisms in response to cravings or triggers. The impaired executive function associated with addiction contributes significantly to the chronic relapsing nature of the disorder.
Therefore, the prefrontal cortex’s role in executive function and decision-making is essential to the science of addiction, particularly in understanding why individuals continue to use drugs despite the obvious harms. Effective treatment strategies must address these cognitive deficits, helping individuals regain control over their impulses and make healthier choices.
Genetic and Environmental Influences on Addiction Vulnerability
Addiction is not simply a matter of willpower or personal choice. Rather, it’s a complex interplay of genetic predispositions and environmental factors that contribute to an individual’s vulnerability. While the science of addiction focuses on neural mechanisms, it’s important to acknowledge the role of both nature and nurture. Genetic factors can influence a person’s sensitivity to the rewarding effects of drugs, their ability to metabolize substances, and their susceptibility to mental health disorders, such as depression and anxiety, which can increase the risk of substance abuse.
The Interaction of Genes and Environment
Environmental factors, such as exposure to stress, trauma, and social influences, also play a significant role in shaping addiction vulnerability. Adverse childhood experiences, such as abuse or neglect, can increase the risk of developing addiction later in life. Similarly, exposure to drug use within the family or peer group can normalize substance abuse and increase the likelihood of experimentation. The availability and accessibility of drugs within a community can also significantly impact rates of addiction. However, it’s important to note that genetics and environment are not mutually exclusive but rather interact in complex ways to influence addiction risk.
For example, an individual with a genetic predisposition to addiction may not develop the disorder if they are raised in a supportive and drug-free environment. Conversely, an individual without a strong genetic predisposition may become addicted to drugs if they are exposed to chronic stress and easy access to substances. Moreover, epigenetic mechanisms, which involve changes in gene expression without altering the underlying DNA sequence, can also play a role in transmitting addiction vulnerability across generations.
Ultimately, the interplay of genetic and environmental factors emphasizes the need for personalized prevention and treatment strategies that address the unique risk factors of each individual. By identifying those at high risk, we can implement early interventions to prevent the onset of addiction and provide targeted support to those who are struggling with substance abuse.
The Role of Neuroplasticity in Addiction Development and Recovery
Neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections throughout life, plays a critical role in both the development of addiction and the potential for recovery. Chronic drug use can induce significant structural and functional changes in the brain, rewiring neural circuits to prioritize drug-seeking behavior. Understanding how neuroplasticity functions is important in the science of addiction: Understanding the neural mechanisms underlying substance abuse.
Brain Remodeling and Addiction
These changes can strengthen the association between drug-related cues and cravings, making it more difficult to resist the urge to use. However, the brain’s capacity for neuroplasticity also offers hope for recovery. Through therapeutic interventions, such as cognitive behavioral therapy and mindfulness-based practices, individuals can learn to rewire their brains and develop healthier coping mechanisms.
By consciously challenging negative thought patterns and behaviors, individuals can strengthen alternative neural pathways that support abstinence and well-being. Furthermore, engaging in activities that promote neurogenesis, such as exercise, learning new skills, and social interaction, can enhance the brain’s ability to repair and adapt. Recovery from addiction is not simply a matter of stopping drug use but rather a process of actively rewiring the brain to support a healthier and more fulfilling life.
- Neuroplasticity enables the brain to reorganize itself by forming new connections.
- Therapeutic interventions can help rewire the brain and promote recovery.
- Engaging in activities that promote neurogenesis can enhance brain repair.
In conclusion, neuroplasticity underscores the dynamic nature of addiction, highlighting the brain’s potential for both positive and negative change. By harnessing the power of neuroplasticity, individuals can overcome addiction and create a more resilient and adaptive brain.
Therapeutic Interventions Targeting Neural Mechanisms of Addiction
Given the complex neural mechanisms underpinning addiction, developing effective therapeutic interventions requires a multifaceted approach to address both the psychological and physiological aspects of the disorder. In light of the science of addiction: Understanding the neural mechanisms underlying substance abuse, various treatments show promise in targeting specific neural pathways involved in addiction.
Treatments and Therapies
Pharmacological interventions, such as medications that block or reduce the effects of drugs, can help to alleviate withdrawal symptoms and reduce cravings. For example, naltrexone, an opioid antagonist, can block the effects of opioids and reduce the rewarding effects of alcohol, while bupropion, an antidepressant, can help to reduce cravings for nicotine and stimulants. Additionally, behavioral therapies, such as cognitive-behavioral therapy (CBT) and contingency management, can help individuals to identify and challenge negative thought patterns and behaviors associated with drug use.
CBT focuses on teaching individuals coping skills to manage cravings, triggers, and stressful situations, while contingency management provides positive reinforcement for maintaining abstinence. Moreover, emerging therapies, such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), are being explored as potential treatments for addiction. TMS involves using magnetic pulses to stimulate specific brain regions, while DBS involves implanting electrodes in the brain to modulate neural activity. These interventions hold promise in directly targeting the neural circuits involved in addiction and restoring normal brain function.
Effective treatment strategies often involve a combination of pharmacological and behavioral interventions tailored to the individual’s unique needs and circumstances. By targeting specific neural mechanisms and addressing the underlying psychological and social factors contributing to addiction, individuals can increase their chances of achieving long-term recovery. Continued research into the neural mechanisms of addiction will pave the way for the development of even more effective and personalized treatments in the future.
| Key Point | Brief Description |
|---|---|
| 🧠 Reward Pathway | Drugs hijack the dopamine system, causing a surge of pleasure. |
| 🥺 Craving & Withdrawal | The amygdala triggers cravings, and withdrawal causes uncomfortable symptoms. |
| 🤔 Executive Function | Substance abuse impairs decision-making and impulse control. |
| 🌱 Neuroplasticity | The brain’s ability to rewire offers hope for recovery through therapy. |
Frequently Asked Questions About Addiction
It’s the study of how drugs affect the brain, causing changes in behavior and leading to compulsive drug-seeking. Scientists explore areas like reward pathways and decision-making circuits.
Drugs cause a massive surge of dopamine, creating an intense feeling of pleasure. This reinforces drug-seeking behavior and can lead to reduced sensitivity to natural rewards.
The prefrontal cortex, responsible for decision-making and impulse control, is weakened by chronic drug use. This leads to impaired judgment and difficulty resisting cravings, driving the cycle of addiction.
Yes, genetics can influence a person’s sensitivity to drugs, how they metabolize substances, and their risk for mental health disorders. However, environmental factors also play a significant role.
Yes, the brain has the capacity to rewire itself through neuroplasticity. Therapeutic interventions, like therapy and exercise, can help strengthen healthier neural pathways and promote recovery from the science of addiction.
Conclusion
In conclusion, the science of addiction: Understanding the neural mechanisms underlying substance abuse reveals a complex interplay of brain regions, neurotransmitters, and genetic and environmental influences. Addiction is a disease that hijacks the brain’s reward system, impairs decision-making, and creates a cycle of craving and dependence. However, with targeted therapeutic interventions and a focus on promoting neuroplasticity, recovery is possible, offering hope for a healthier and more fulfilling life.